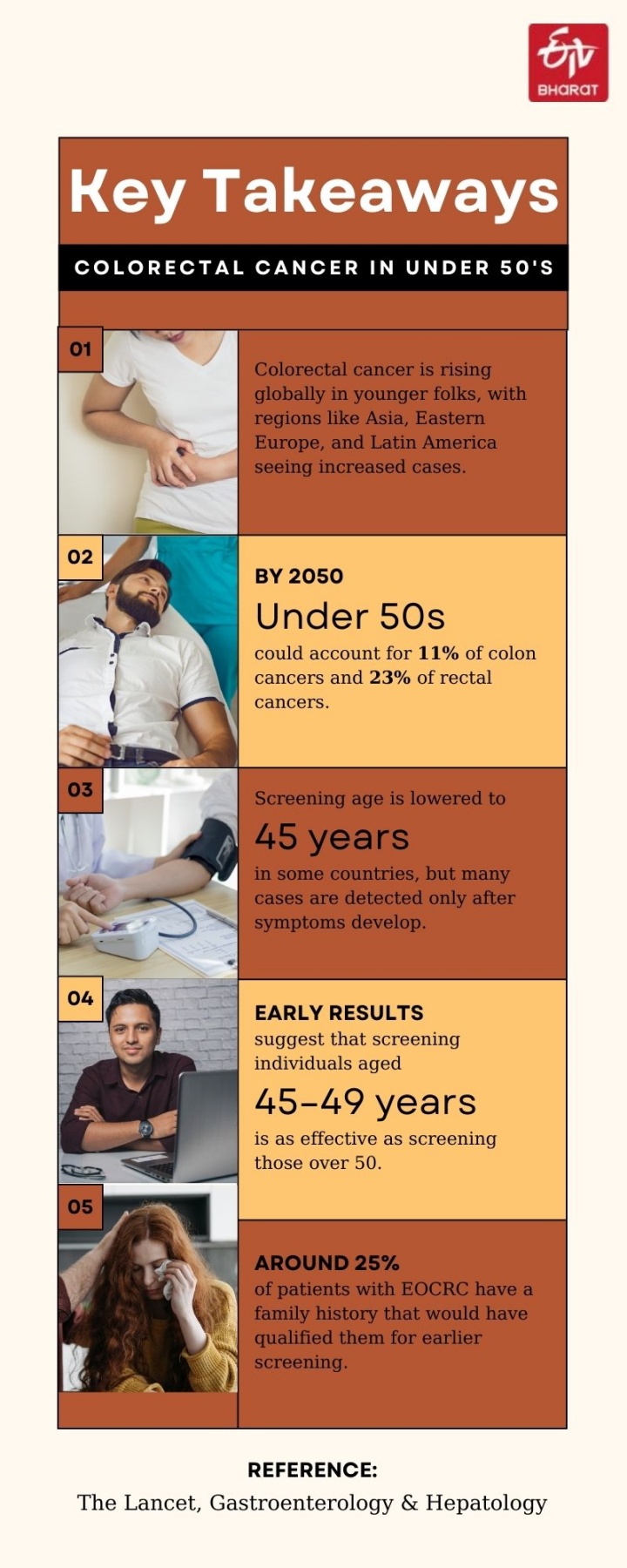
Colorectal cancer, often associated with older adults, is increasingly affecting younger populations across the globe. A growing number of cases are being reported in individuals aged 25 to 49, with regions like Eastern Europe, Asia, and Latin America joining Western countries in experiencing a surge.
For instance, Australia, Puerto Rico, New Zealand, the USA, and South Korea report the highest early-onset colorectal cancer (EOCRC) rates. By 2030, an estimated 11% of colon cancers and 23% of rectal cancers will occur in individuals under 50.
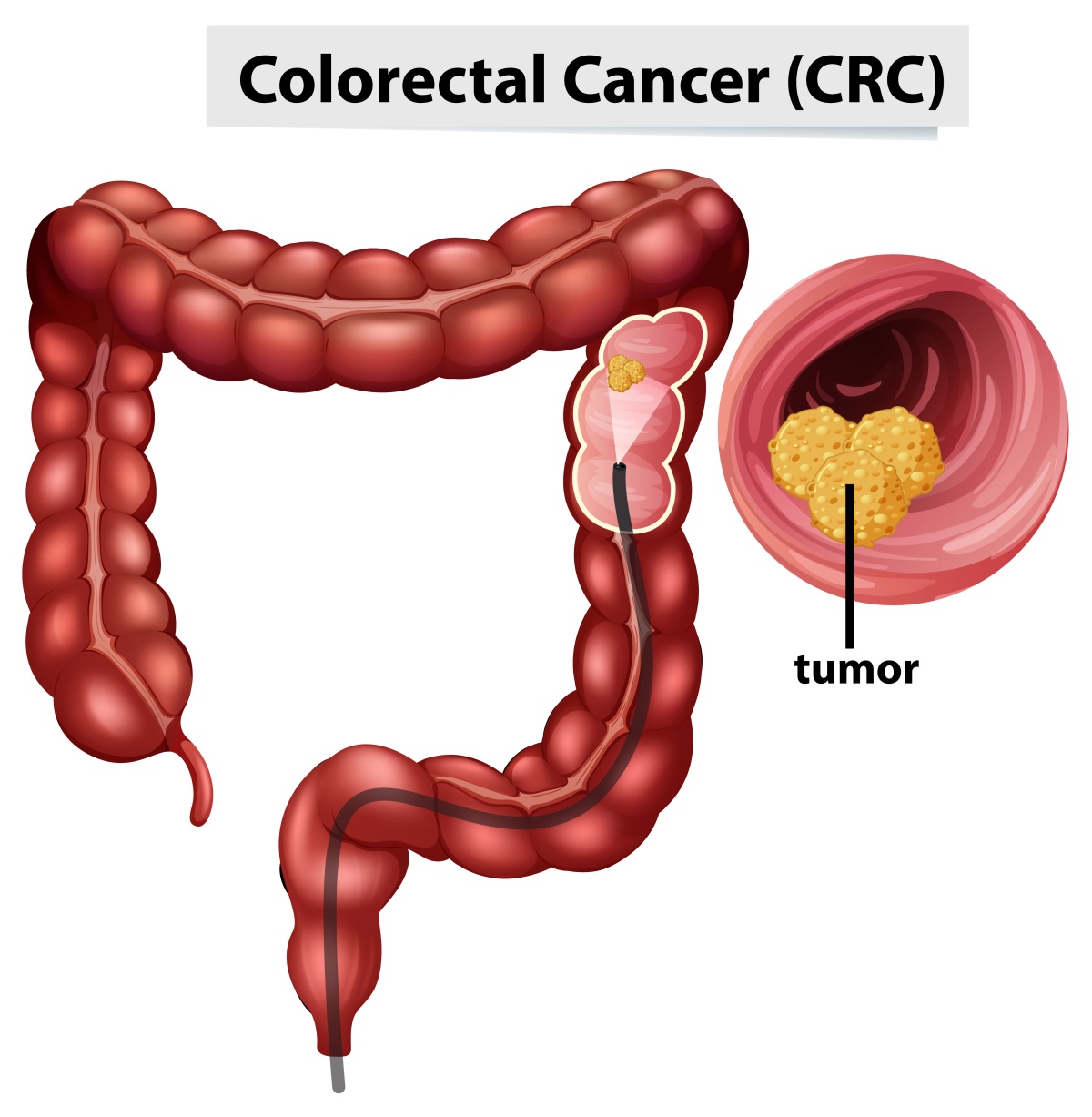
What Is Colorectal Cancer?
Colorectal cancer is a type of cancer that starts in the colon (large intestine) or rectum, which are key parts of the digestive system. It usually begins as small growths called polyps on the inner lining of the colon or rectum. Over time, some of these polyps can turn into cancer. The disease can cause symptoms like changes in bowel habits, blood in stool, abdominal pain, or weight loss, but it often develops silently in its early stages. Early detection through screenings, like colonoscopies, is crucial because colorectal cancer is highly treatable when caught early.
What’s Behind the Rise?
One in six people diagnosed with EOCRC has a genetic mutation linked to cancer risk. However, genetics alone cannot explain the rapid increase, as they are unlikely to have changed significantly in recent decades. Instead, experts believe a “birth cohort effect” may be at play, with individuals born after 1960 exposed to environmental and lifestyle factors that elevate risk.
Factors like obesity, metabolic syndrome, sedentary lifestyles, alcohol consumption, Western diets, and even antibiotic use are suspected contributors. However, these associations remain mixed, making it challenging to identify risk factors beyond genetics and family history for targeted screening.
Catching Cancer Earlier
In response to rising EOCRC rates, some countries have lowered the recommended age for colorectal cancer screening. The US reduced its starting age from 50 to 45 in 2018, and Australia followed suit in 2024 for its national bowel cancer screening program. Early results suggest that screening individuals aged 45–49 is as effective as screening those over 50.
However, the expanded guidelines have sparked debate, with concerns about diverting resources away from higher-risk populations. Despite these changes, most EOCRC cases are detected only after symptoms appear, often at advanced stages. Around 25% of patients with EOCRC have a family history that would have qualified them for earlier screening.
New Challenge for Clinicians
Doctors are now seeing a younger demographic of colorectal cancer patients with unique challenges. Symptoms in younger individuals are often dismissed or misdiagnosed as less serious conditions, delaying timely diagnosis. General practitioners report difficulties in distinguishing cancer symptoms from benign issues and fear over-referring patients for further tests.
The belief that colorectal cancer is a disease of the elderly must change, as earlier recognition is key to improving outcomes. Treatment for EOCRC is typically aggressive, but the survival benefit is often minimal. Moreover, younger patients face long-term psychosocial challenges, including anxiety, body image concerns, and worries about bowel, urinary, or sexual dysfunction post-treatment.
Emotional Toll On Younger Patients
For those under 50, the impact of EOCRC extends beyond physical health. Many are in the prime of their lives, balancing careers, education, and family responsibilities. Younger patients often report higher levels of anxiety, worsened body image, and significant concerns about long-term treatment side effects. Holistic care that addresses these challenges is crucial.
Read more:



