By Aparna Roy, Fellow & Lead, Climate Change and Energy, ORF
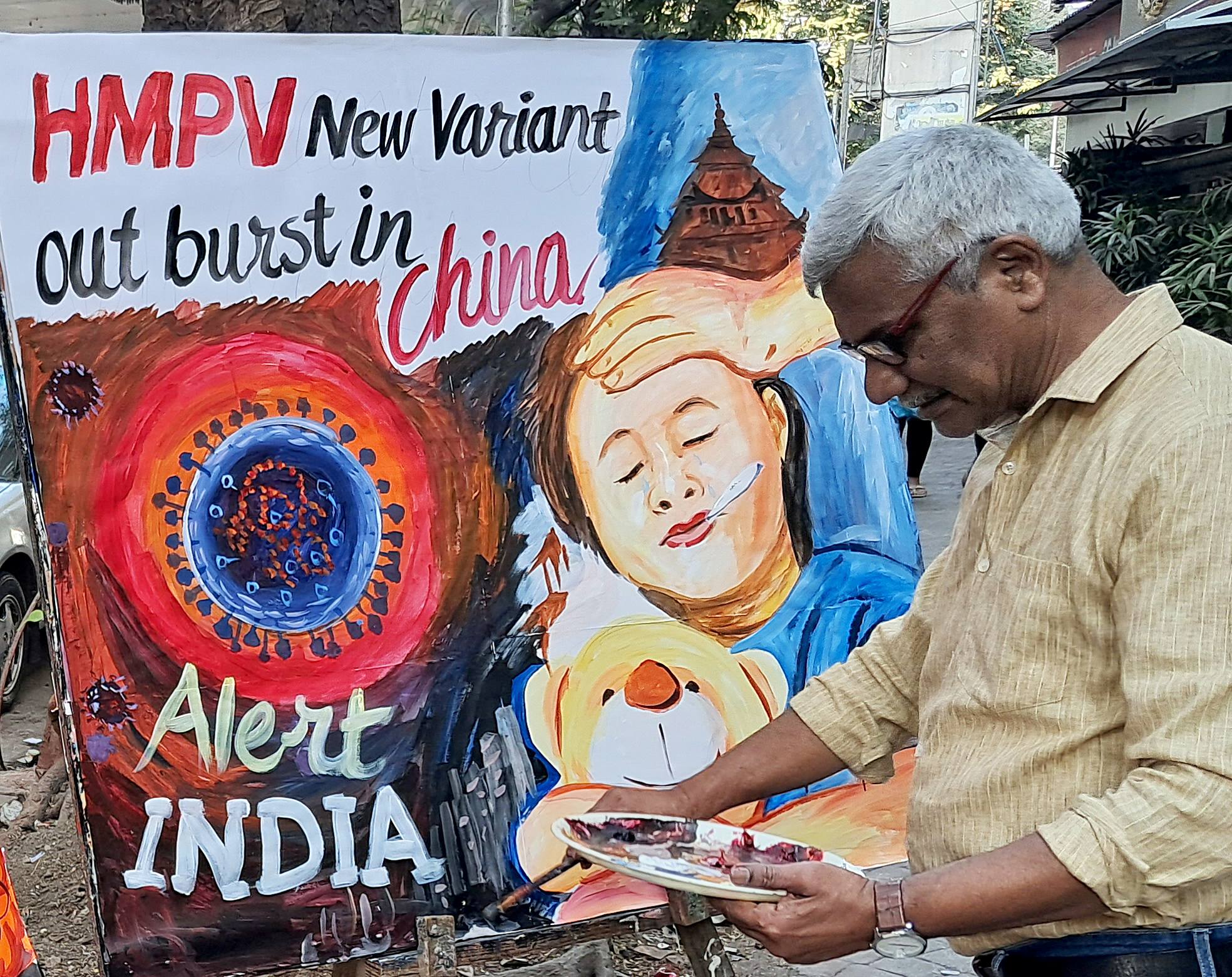
The recent outbreak of Human Metapneumovirus (HMPV) in China has given India reasons to be wary. Although HMPV has been in circulation in India since 2001 and has not yet triggered a large-scale public health emergency, recent data suggests a troubling rise in infections. The Centers for Disease Control and Prevention (CDC) reported a 36% rise in HMPV detections in 2024, with hospitals witnessing increased admissions, particularly among children and the elderly.
Typically causing flu-like symptoms, this virus can lead to severe respiratory distress, especially in children, the elderly, and immunocompromised individuals. However recent studies highlight an even alarming trend: the incidence and severity of such infections are exacerbated by climate change.

Climate change is reshaping the epidemiology of infectious diseases, creating conditions ripe for their spread. Rising temperatures, erratic weather patterns, and increased humidity create favourable environments for viral persistence and transmission. For instance, warmer winters and prolonged rainy seasons—hallmarks of India’s changing climate—are associated with longer periods of viral activity, overwhelming public health systems.
HMPV, like many respiratory viruses, thrives in these shifting environmental conditions. Research published in Nature Climate Change indicates that changes in seasonal cycles due to global warming are altering virus transmission windows, leading to off-season outbreaks and compounding health risks. Vulnerable populations in urban slums, rural areas, and regions experiencing frequent climate disasters face disproportionate impacts due to overcrowding, poor sanitation, and limited healthcare access.

Despite these clear links, India’s public health response to HMPV and similar diseases rarely integrates climate change into its framework. National programs like the Integrated Disease Surveillance Programme (IDSP) are designed to monitor infectious diseases but often fail to address the environmental stressors that drive outbreaks. Similarly, while India’s National Action Plan on Climate Change and Human Health (NAPCCHH) mentions climate-sensitive illnesses, it lacks specific strategies to tackle respiratory viruses such as HMPV.

Stepping up surveillance at the states as case rises, would not lead to an effective outcome. India needs to urgently adopt an aggressive strategy that integrates climate resilience and disaster response policies into all aspects of HMPV prevention and control response strategies, including monitoring, diagnosis, and infrastructure while addressing financial, technical, and capacity gaps.
Currently, policies addressing infectious diseases and climate change in India operate in silos, leading to fragmented strategies that fail to address their intricate relationship. For instance, while health programs such as the National Programme on Climate Change and Human Health (NPCCHH) under the National Health Mission focus on strengthening the healthcare system to reduce illnesses caused by climate change, it overlooks the broader climatic factors—such as rising temperatures, erratic rainfall, and prolonged humidity—that exacerbate the spread and persistence of respiratory viruses like HMPV. Similarly, states’ climate action plans rarely incorporate health-specific interventions, creating a critical gap in coordinated response mechanisms.
A key challenge in developing an effective climate-resilient health strategy lies in the lack of a comprehensive database linking climate variables with disease prevalence across regions. Most states lack integrated climate-health surveillance systems that can track the interaction between environmental conditions and the spread of respiratory illnesses. Without this critical data, it becomes nearly impossible to predict outbreak patterns, allocate resources efficiently, or develop targeted crisis response mechanisms for at-risk populations.
By leveraging advancements in home-based digital health technologies, India can revolutionise its health crisis response. Wearable physiological sensors, Smart inhalers and purpose-built smartphone apps like the AERIAL TempTracker, can generate real-time data that informs adaptive respiratory health strategies in the face of changing climate patterns. Given the urgency to address the potential HMPV outbreak across India, it is imperative for India to foster advanced research facilities capable of developing predictive analytics using artificial intelligence and health informatics that could help identify hotspots for HMPV outbreaks based on climate variables, guiding pre-emptive interventions.
Transforming health care from reactive, post-incident treatment to proactive prevention of diseases demands a robust implementation on the ground. India’s existing infrastructure struggles to meet even routine demands, let alone climate-driven health emergencies. India has only 0.5 hospital beds per 1,000 people and just one doctor for every 1,511 individuals. The shortage of healthcare professionals is particularly acute in rural areas, where there are only 3.2 government hospital beds per 10,000 people.
This systemic inadequacy leaves India ill-equipped to handle the added burden of virus outbreaks like HMPV. Expanding healthcare facilities, particularly in underserved rural areas, and investing in training medical staff to recognize and treat climate-sensitive illnesses are critical first steps. Targeted programs to equip district hospitals with advanced diagnostic tools can further enhance preparedness for the escalating health challenges.
Lastly, addressing climate-induced respiratory health challenges requires a collaborative approach that go beyond government efforts alone. Just as ASHA workers have played a pivotal role in maternal and child health, a similar cadre of community health responders could be mobilized to tackle viral outbreaks. These responders, trained to identify early signs of respiratory distress linked to climate factors, would serve as frontline support in vulnerable regions, bridging gaps in access to care.
HMPV may be just one virus, but it symbolizes a larger trend of climate-sensitive health crises that will only grow more severe. By prioritizing climate resilience in public health planning, India has an opportunity to safeguard its citizens from the cascading impacts of a warming world.
(Disclaimer: The opinions expressed in this article are those of the writer. The facts and opinions expressed here do not reflect the views of ETV Bharat)



