The normal tendency is people are going to be naïve if they are not going to be explained properly at the time of discharge as to what is to be done and what is not to be done predominantly the hospital admissions tend to be due to lung involvement and they are discharged once their oxygen levels are stable at 90-92 %. this cannot be discounted in terms of patient education because they need to monitor their oxygen levels at home with support and physiotherapy assistance. when it is missed out, they tend to develop hypoxemia which plays a crucial role in their brain functionality. This hypoxemia presents as drowsiness, delirium, unable to check things properly.
The second scenario is people go home maintain oxygen on some kind of oxygen support or an oxygen concentrator but they tend to forget that once they start walking they tend to lose more oxygen, hypoxemia ensues.
Another important factor seen in recovery is sugar control. Diabetes played havoc in terms of COVID. Blood sugar whether high or low, definitely impacts the concentration levels of the brain. So it is important that people monitor their sugars as the levels tend to be very erratic especially with steroids going on due to the inflammation ongoing in the body. As the inflammation comes down the sugars also vary. Likewise, if the doses are going to be optimized then it takes care of the situation. When there is a failure of optimization of sugar levels, then there is a fear of hypoglycemia.
Similarly, if there is a failure to recognize that the patient has developed diabetes, then hyperglycemia can occur which can also cause problems with the brain. These uncontrolled levels can lead to a brain stroke. So, the brain functions may be compromised and cause electrolyte disturbances.
Another important thing is low sodium level. This can happen due to drugs and also the hydration status of the brain. Another fact to be considered is that these patients come with a lot of comorbid conditions like hypertension, epilepsy, neuropathy and the patient may be on long-term medications and these medicines need to be restored when discharging the patient.
Holistically when the patient gets discharged, appropriate assessment needs to be done and accordingly the advice has to be given.
Many people have had a tube due to a ventilator or have had intubation done, these people tend to have an issue with their voice. Fortunately, the ventilation part for COVID has been short-lived as COVID is a disease of only 2 weeks duration and those who have had damage to their vocal cords due to ventilation, have a harsh voice, weak voice. it is important to contact your healthcare professional if recovery is too slow or there is a deterioration in your condition.
Also Read: Post-COVID Lung Care and Rehabilitation
WHO advises Post COVID Voice Care:
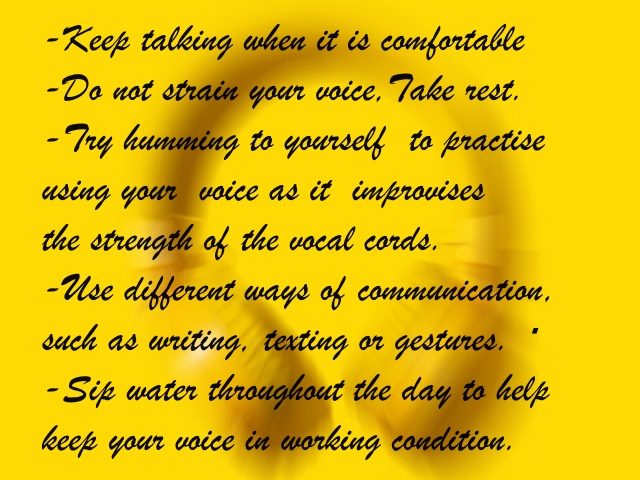
It is best to have a graded use of voice on the advice of a speech therapist. Intensive spirometry helps to strengthen vocal cords and so also does steam inhalation. Patients still have some amount of difficulty with some syllables. A graded approach may help them regain their voice over a period of time.
Managing daily activities; Patients feel they are alright and the acceptance of the fact that it's going to take time to adjust to your daily routine needs to be stressed upon. The patients would be requiring 6 weeks to recover to do only those activities which do not cause any breathlessness.
It is important to maintain some healthy habits
- Maintain adequate rest.
- Sleep for 7-8 hours at a more or less fixed time from 10 or 11 pm to about 6- am in the morning. This is very important as it gives them the required energy to perform their daily activities.
- Some amount of minimal exercises but no rigorous exercises.
- An adequate amount of hydration is of foremost importance as many people tend to miss out on this. At least 2-3 liters of water a day in this weather is recommended.
- A good amount of breakfast, containing protein-rich foods, less on fats and still less on carbohydrates. This should be on the advice of your doctor.
- One may take help from a professional nutritionist in planning your diet. All the zinc and vitamin C requirements can be consumed from natural foods instead of supplements.
- Instead of idling away their time sitting around, a gentle walk is advised.
For your queries, contact Dr. Rajesh Vukkala at vukkala@gmail.com



