Cambridge (England): People often jokingly say they've got a bit of OCD (obsessive-compulsive disorder) if they are overly organised or tidy. But OCD is actually a severe and disabling disorder characterised by obsessions recurrent intrusive thoughts, impulses or images that are unwanted and anxiety provoking. This is often coupled with compulsions, which are ritualistic mental or physical actions.
Some people with OCD are engaged in rituals for much of their waking life and cannot even leave their homes. As the condition is difficult to treat, life with OCD can be extremely difficult. But in our new research, published in Nature Communications, we discovered an imbalance in brain chemicals in OCD that could lead to radically different and improved treatments.
OCD affects around 3% of the population. The average age of onset is 19.5 years, which means that many cases go undetected in childhood and adolescence. NHS-recommended treatments include cognitive behavioural therapy and antidepressant drugs called selective serotonin re-uptake inhibitors (SSRIs), which boost the chemical serotonin in the brain. However, 50% of OCD patients don't respond fully to SSRIs meaning their symptoms are likely to continue to some extent. And at least eight weeks of sustained treatment is typically needed before any meaningful clinical improvement can be seen.
To be able to develop more effective treatments, it is crucial that we understand the chemical basis of OCD in the brain. Scientists have suspected that this involves an imbalance between chemical messengers, or neurotransmitters, called glutamate and gamma-aminobutyric acid (Gaba) in certain brain regions.
While glutamate promotes communication between neurons, Gaba reduces or inhibits neural communication (calming the central nervous system and making us less inhibited). Imbalances in these chemicals can therefore make communications more or less difficult within neural circuits in the brain potentially leading to symptoms such as compulsions and intrusive thoughts.
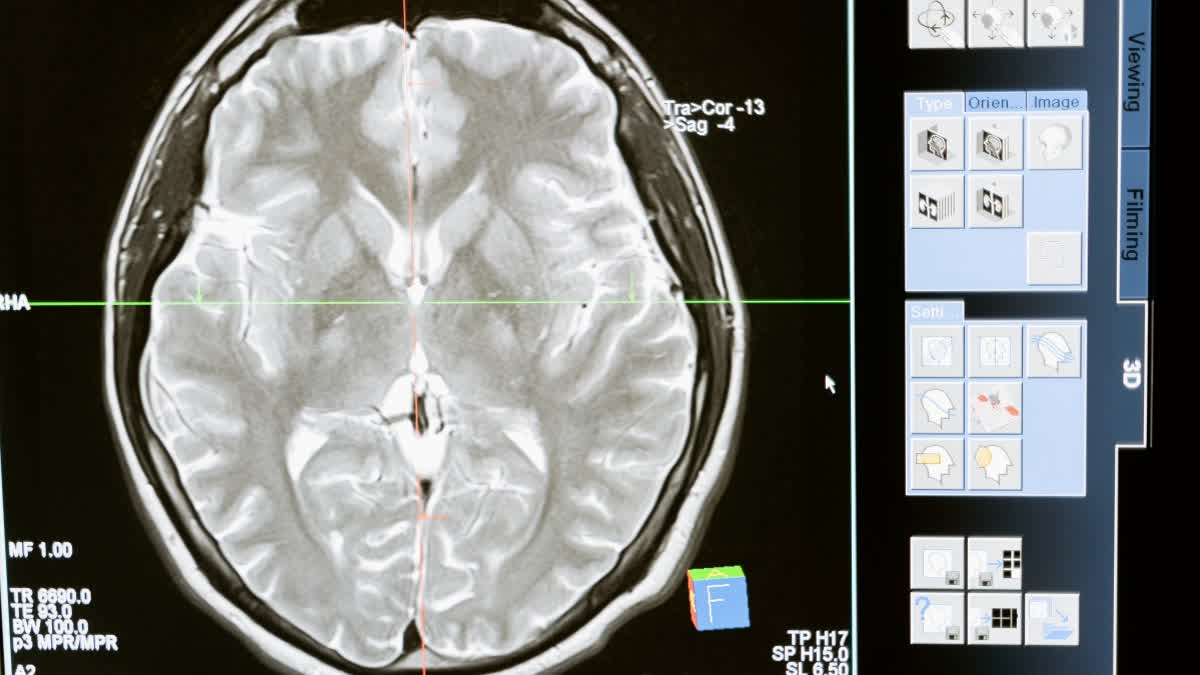
Magnetic resonance spectroscopy: To study glutamate and Gaba, we used a high-strength magnet (called 7-Tesla) to perform magnetic resonance spectroscopy. This technique detects radio frequency electromagnetic signals produced by the atomic nuclei in molecules. This helps scientists to measure what kind of chemicals exist there and their concentration. This allowed us to detect and measure glutamate and Gaba levels separately in different brain regions. We specifically looked at two brain regions toward the front of the brain called the anterior cingulate cortex (ACC) and the supplementary motor area (SMA).
Also read: Performing arts may help in lowering anxiety and depression: Study
That's because previous studies had already shown that these areas, involved in actions, are affected in OCD. Activity in the ACC changes in response to reward or punishment, guiding future decision-making. The SMA is involved in the coordination of motor sequences and seems to have a role in the production of habits.
We found an imbalance between glutamate and Gaba levels in a group of 31 patients with OCD in the frontal regions of the brain. Specifically, OCD patients had increased levels of glutamate and lower levels of Gaba in the ACC. This means that they had very high levels of neural communication in the area, potentially making it hyperactive. They also had a disrupted balance between these chemicals in the SMA.
Importantly, the clinical severity of compulsive symptoms of OCD correlated with the glutamate levels we measured in the SMA. Self-rated questionnaires of compulsive tendencies by both people with OCD and those in a healthy volunteer control group also correlated with glutamate in this region. For the ACC, we found that that people's proneness to habit (which is closely linked to compulsion) correlated with the glutamate/Gaba balance that we discovered.
Future treatments: The finding raises hopes for better treatments for OCD, focusing on re-balancing glutamate and Gaba levels in key brain regions. Some genetic evidence also suggests that the genes of people with OCD that regulate glutamate levels in the brain may be impaired.
One possible approach is to use drugs that reduce the release of glutamate from nerve cells at certain receptors in the brain (known as metabotropic glutamate 2 receptors). These are receptors that glutamate binds to, they suppress activity in the nerve cells that use it as a chemical transmitter. One such existing class of drugs works on this receptor and has already been tried safely in humans. However, these drugs have not yet been trialled in patients with OCD.
In patients with extremely severe OCD, for whom all other usual treatments have failed, surgeons have actually removed the ACC. This is one of the very few examples of where psychosurgery has been shown to be beneficial with few reported adverse effects on cognition. In the future, though, rather than removing the ACC in such patients, deep brain stimulation through implanted electrodes could be used to reduce activity in this region.
And for less severely impaired patients where such drastic treatments are not justified, there may be therapeutic possibilities of using transcranial magnetic stimulation. This treatment is administered via a magnetic coil positioned against the scalp to readjust the chemical balance and activity of these neural circuits. In future, if OCD is diagnosed early in the course of the illness and the chemical imbalance we have discovered is also detected then these new treatments offer hope for improved quality of life and wellbeing for patients the disorder. (PTI)