Mumbai (Maharashtra): Mucormycosis also known as 'Black Fungus' is a rare fungal infection that is spreading its tentacles in the state. There are about 2,000 active mucormycosis cases in the state and 10 people have already succumbed to the fungal infection. It is particularly being diagnosed in patients who have recovered from Covid.
Some patients have even lost their eyesight due to this, as informed by the central government's Health and Family Planning Department. The department has also released information about how people get infected and how is it related to Covid, its symptoms, treatment and precaution.
How does a person get infected with mucormycosis?
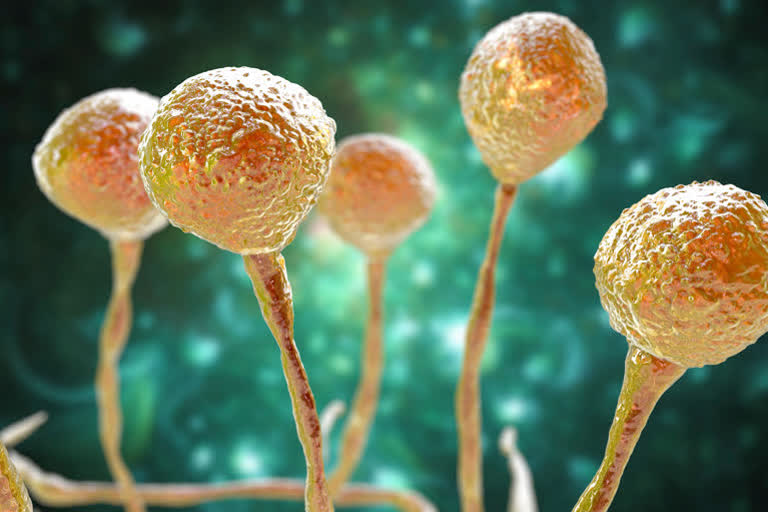
It is a fungal infection. The fungus enters the body through cuts, scratches, burns or wounds. According to the Indian Council for Medical Research (ICMR) diabetes, use of steroids which weaken the immune system, prolonged hospitalization, organ transplant, tumour, presence of cancer cells increases the risk of mucormycosis.
It is commonly called a black fungus. When an individual comes in contact with fungal spores in their environment they get infected. It is present in the environment, particularly in mud, leaves, fertilizers and putrified material. Covid patients and diabetics are more vulnerable. Not only Covid patients but diabetics with low immunity are prone to get infected.
Read: Patole seeks probe into 'phone-tapping' during previous govt
The natural immune system is capable of defeating this fungus but some medicines given to Covid patients which suppress their natural immunity make them prone to fungal infection. Patients recovering in the intensive care units are likely to catch due to the humidity in the ICU. It is a rare disease which if not treated in time can be fatal.
Common symptoms of mucormycosis
Mucormycosis first infects the sinus and spreads to the teeth and later attacks the eyes. In the later stage, it affects the lungs and brain. Black dots are seen on the face and nose of the patients, vision diminishes, pain in the chest, trouble in breathing, blood coming out with cough are some of the symptoms.
However, experts warn that one should not confuse regular cold with fungal infection. Particularly Covid patients undergoing treatment or those who have recovered should be careful about the symptoms. Medical tests and expert advice are necessary to confirm mucormycosis.
How to treat mucormycosis?
Though it starts with a skin infection it can spread to other parts of the body. During the treatment, the dead and infected tissues have to be removed. So some patients lose the upper jaw or an eye. Treatment also includes 4-6 weeks of intravenous anti-fungal treatment to remove the infection.
Read: 4-yr-old Pari defeats Covid, fight with cancer continues
It affects the whole body and therefore a team comprising a microbiologist, intensive neurologist, ear-nose-throat specialist, opthalmologist, dentist, surgeon, and other experts are involved in the treatment.
Prevention of mucormycosis
Diabetics should be particularly careful. Keeping diabetes in control is the first prevention, according to ICMR. Self-medication and overuse of steroids can be dangerous. It is advisable to follow doctors' prescriptions.
Invalid use of steroids can be fatal
Regarding steroids, NITI Aayog (Health) member Dr VK Paul said that it should not be used in the initial stages of Covid treatment. Patients should take medicines prescribed by the doctor and only for the period that the doctor has suggested. Medicines taken for a longer duration than required can have ill effects.
Fungal infection due to low immunity
Besides steroids, medicines like Tocilizumab and Itolizumab too affect the immune system. It is known that Corona can cause multi-organ failure in some cases. If these medicines are used improperly it can weaken the immunity.
Read: Maharashtra cancels class 10 board exams
ICMR has directed the concerned to stop the use of immunomodulating drugs which damages the immunity. Covid Task Force has improved the dose of tocilizumab to avoid ill effects which may weaken the person's immune system.
Proper hygiene can also help avoid the disease
Patients on oxygen should be careful. The humidifiers used by patients on oxygen should be regularly cleaned and ensure that clean water is used. Leakage of water should be avoided to avoid the growth of fungus. Patients should wash their hands from time to time and should follow hygiene, said Dr Paul.
Precaution important after cure
Covid patients who have recovered should look for symptoms and be careful. Symptoms should not be ignored as the infection is found in patients a few weeks after recovery or a few months after recovery. Timely detection helps in the early cure of the fungal infection. Medicines should be taken only with the doctor's advice.