Mumbai: With the National Democratic Alliance government bracing towards presenting its first budget in its second term, there is an overall enthusiasm on the allocations of budget to the health sector, given its importance as one of the key social indicators of country’s development.
India spends nearly 1.4 per cent of its GDP, which is lesser than the spending of the developing countries like Sri Lanka (1.6 per cent) and Bhutan (2.5 per cent) on the health sector.
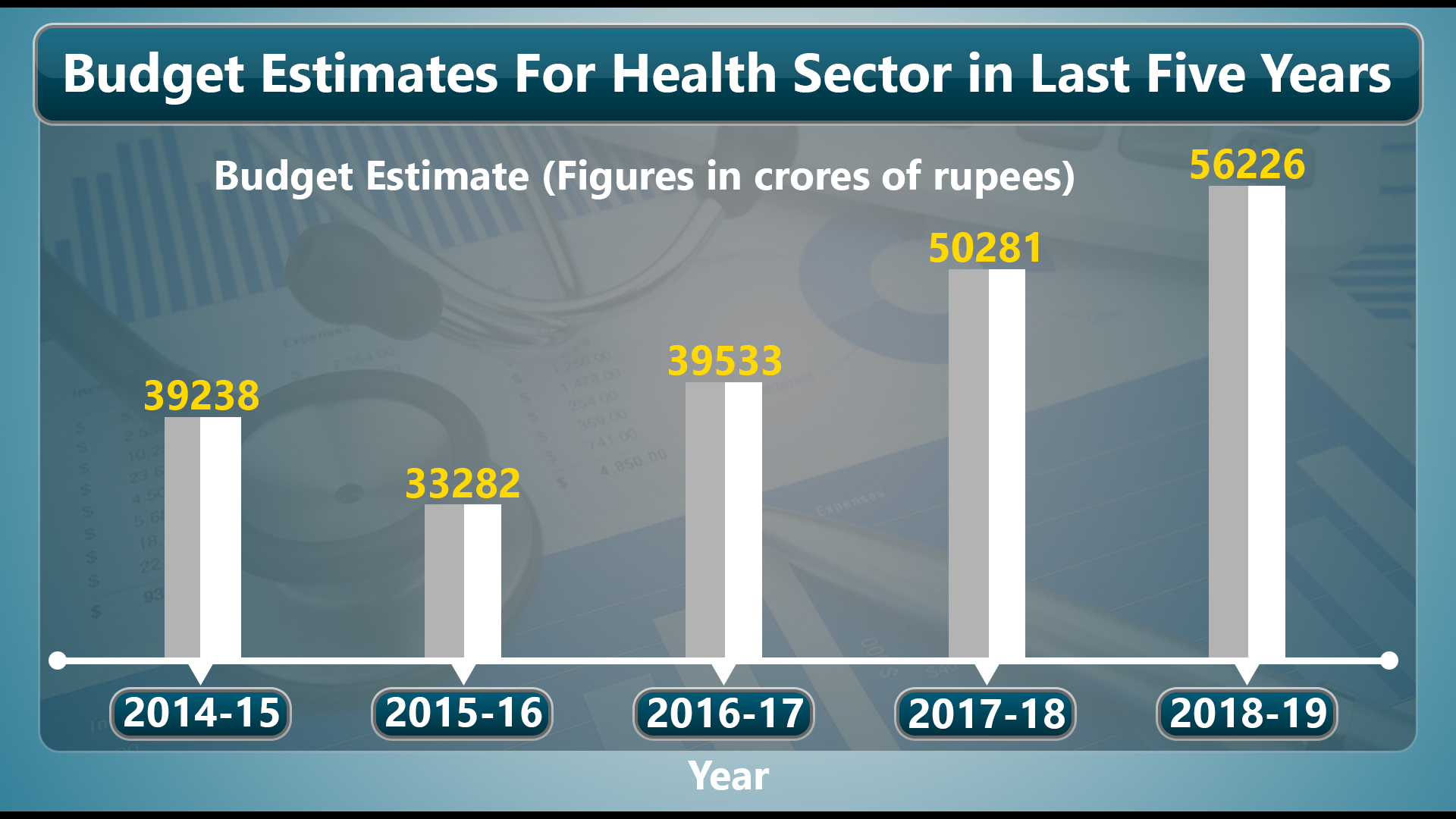
One positive development in the recent past is that the budget allocations to the health sector increased significantly in the interim budget for 2019-20, presented during the regime of NDA-1. An amount of Rs. 61, 398 crores was allotted to the health sector in the interim budget, which is 16.3 per cent higher than the previous year’s allocation for the same.
However, these allocations need to have a much more balanced approach. For instance, there is an exponential increase of budgetary allocations to Ayushman Bharat Yojana in the interim budget, which increased by 166 per cent when compared to the allocation it got in the last financial year.
Read more:India fast becoming hub of spurious cigarette manufacturing in world
At the same time, the budget for the flexi pool for non-communicable diseases, injury and trauma, National Programme for Prevention and Control of Cancer, diabetes, cardiovascular disease and stroke had to suffer cuts. These are the key areas of the health sector that indeed needs larger attention and higher allocations.
While Ayushman Bharat Yojana is a noble initiative aimed at providing free insurance of Rs. 5 lakh per family to nearly 40 per cent of the country’s population, it is equally important to give due attention needed to other key schemes and areas of India’s health sector.
Shortage of health infrastructure
There is a serious shortage of health infrastructure that craves for attention. According to Rural Health Statistics of 2016, there is a 22 per cent shortage of primary health centres, 20 percentage shortage of health sub-centres and 30 per cent shortage of community health centres across the country.
More importantly, the population-doctor ratio in the country’s government hospitals is 25 times lower than the ratio that has been recommended by the World Health Organization.
Requirement of larger budgetary allocation
Improving on these fronts require larger budgetary allocation with consistent monitoring and supervision. There are other areas of concern like, maternal mortality rates and the infant mortality rates, where poor countries like Rwanda and Ethiopia offers great lessons with minimum expenditure.
Link accountability of health care workers with incentives
Rwanda attempted to link accountability of health care workers with incentives. They were offered some incentives in monetary form, for adhering to the clinical guidelines. As a result, their performance improved significantly. At the same time the government there, improved access to information about the quality of local health services in Rwanda to the rural populations, which in turn increased public awareness.
Trained health extension workers
Even Ethiopia stood as an example of accomplishment in improving its health care status. It trained thousands of health extension workers and rural high school graduates for a year. Later, they were sent back to their local areas. As a result, they were able to reduce the child mortality rates by 32 per cent and maternal mortality rates by 38 per cent.
Allocations in India’s budget, exclusively, to such initiatives on the lines of these poor countries, could go a long way in improving the health sector’s performance to a large extent.
(Written by Dr. Mahendra Babu Kuruva, Assistant Professor at H.N.B. Garhwal Central University, Uttarakhand)



