Hyderabad: The COVID-19 pandemic has severely disrupted the prevention and treatment services for noncommunicable diseases (NCDs), a WHO survey released today has found. The survey, which was completed by 155 countries during 3 weeks in May, confirmed that the impact is global, but that low-income countries are most affected.
This situation is of significant concern because people living with NCDs are at higher risk of severe COVID-19-related illness and death.
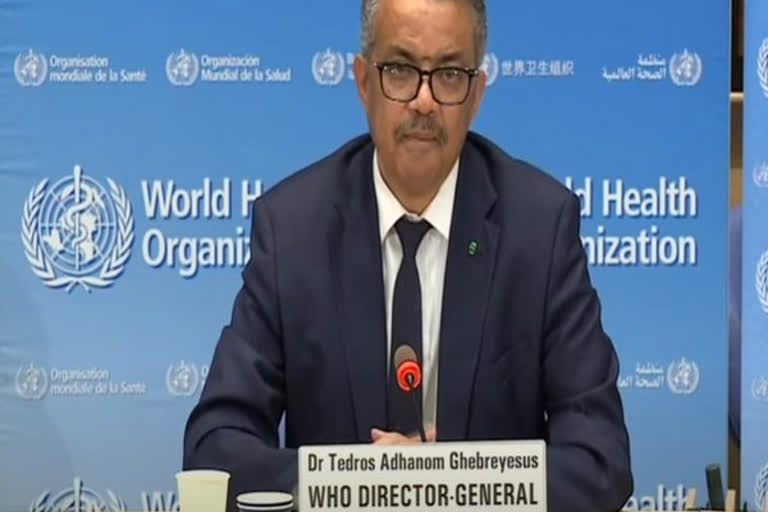
“The results of this survey confirm what we have been hearing from countries for a number of weeks now,” said Dr Tedros Adhanom Ghebreyesus, Director-General of the World Health Organization.
“Many people who need treatment for diseases like cancer, cardiovascular disease and diabetes have not been receiving the health services and medicines they need since the COVID-19 pandemic began. It’s vital that countries find innovative ways to ensure that essential services for NCDs continue, even as they fight COVID-19.”
Service disruptions are widespread
The main finding of the survey is that health services have been partially or completely disrupted in many countries. More than half (53%) of the countries surveyed have partially or completely disrupted services for hypertension treatment; 49% for treatment for diabetes and diabetes-related complications; 42% for cancer treatment, and 31% for cardiovascular emergencies.
Also read: Community transmission of coronavirus infection well-established: experts
Rehabilitation services have been disrupted in almost two-thirds (63%) of countries, even though rehabilitation is key to a healthy recovery following a severe illness from COVID-19.
Reassignment of staff and postponing of screening
The survey has found that in the majority (94%) of countries responding, ministry of health staff working in the area of NCDs were partially or fully reassigned to support COVID-19.
The postponement of public screening programmes (for example for breast and cervical cancer) was also widespread, reported by more than 50% of countries. This was consistent with initial WHO recommendations to minimize non-urgent facility-based care whilst tackling the pandemic.
But the most common reasons for discontinuing or reducing services were cancellations of planned treatments, a decrease in public transport available and a lack of staff because health workers had been reassigned to support COVID-19 services. In one in five countries (20%) reporting disruptions, one of the main reasons for discontinuing services was a shortage of medicines, diagnostics and other technologies.
Unsurprisingly, there appears to be a correlation between levels of disruption to services for treating NCDs and the evolution of the COVID-19 outbreak in a country. Services become increasingly disrupted as a country moves from sporadic cases to community transmission of the coronavirus.
Globally, two-thirds of countries reported that they had included NCD services in their national COVID-19 preparedness and response plans; 72% of high-income countries reported inclusion compared to 42% of low-income countries. Services to address cardiovascular disease, cancer, diabetes and chronic respiratory disease were the most frequently included. Dental services, rehabilitation and tobacco cessation activities were not as widely included in response plans according to country reports.
Also read: Celltrion announces positive pre-clinical results for COVID-19 antiviral antibody treatment
Seventeen percent of countries reporting have started to allocate additional funding from the government budget to include the provision of NCD services in their national COVID-19 plan.
Alternative strategies for continuing care being implemented
Encouraging findings of the survey were that alternative strategies have been established in most countries to support the people at the highest risk to continue receiving treatment for NCDs. Among the countries reporting service disruptions, globally 58% of countries are now using telemedicine (advice by telephone or online means) to replace in-person consultations; in low-income countries, this figure is 42%. Triaging to determine priorities has also been widely used, in two-thirds of countries reporting.
Also encouraging is that more than 70% of countries reported collecting data on the number of COVID-19 patients who also have an NCD.
”It will be some time before we know the full extent of the impact of disruptions to health care during COVID-19 on people with noncommunicable diseases,” said Dr Bente Mikkelsen, Director of the Department of Noncommunicable Diseases at WHO.
Also read: PM Modi 'indispensable' leader but how to rectify mistakes, asks Shiv Sena
“What we know now, however, is that not only are people with NCDs more vulnerable to becoming seriously ill with the virus, but many are unable to access the treatment they need to manage their illnesses. It is very important not only that care for people living with NCDs is included in national response and preparedness plans for COVID-19 -̶ but that innovative ways are found to implement those plans . We must be ready to “build back better” ̶ strengthening health services so that they are better equipped to prevent, diagnose and provide care for NCDs in the future, in any circumstances,” said Dr Bente.