With the World Health Organization (WHO) declaring MPox a global public health emergency (PME), twice within a space of two years, alarm bells are ringing across the world. With neighbouring Pakistan also reporting four cases, there is understandable concern about India’s vulnerability to the possible entry into India and potential spread across a vast population most of which has no previously acquired immunity.
The Government of India has initiated heightened surveillance measures for any outbreak and ordered screening of travellers entering Indian airports and seaports from any affected country.
Even as we gear up our public health defences, there are several questions which need clarification in the public mind. What is the correct name - Mpox or monkeypox? How is it different from chicken pox or smallpox? Where did the virus originate? How did humans get infected from animals? How does it spread from human to human? What personal precautions must be taken to protect oneself, if there is an outbreak in India or while travelling to an affected country? Is there a vaccine which protects against the disease? Are drugs available to treat the disease? It is incorrect to use the name monkeypox. That name was originally given because a German laboratory first identified the virus in monkeys imported from Singapore. However, the virus mostly spreads to humans from rodents like rats and squirrels. Because of the misleading association of human infection with monkeys, the stigmatising name was changed to Mpox by WHO.
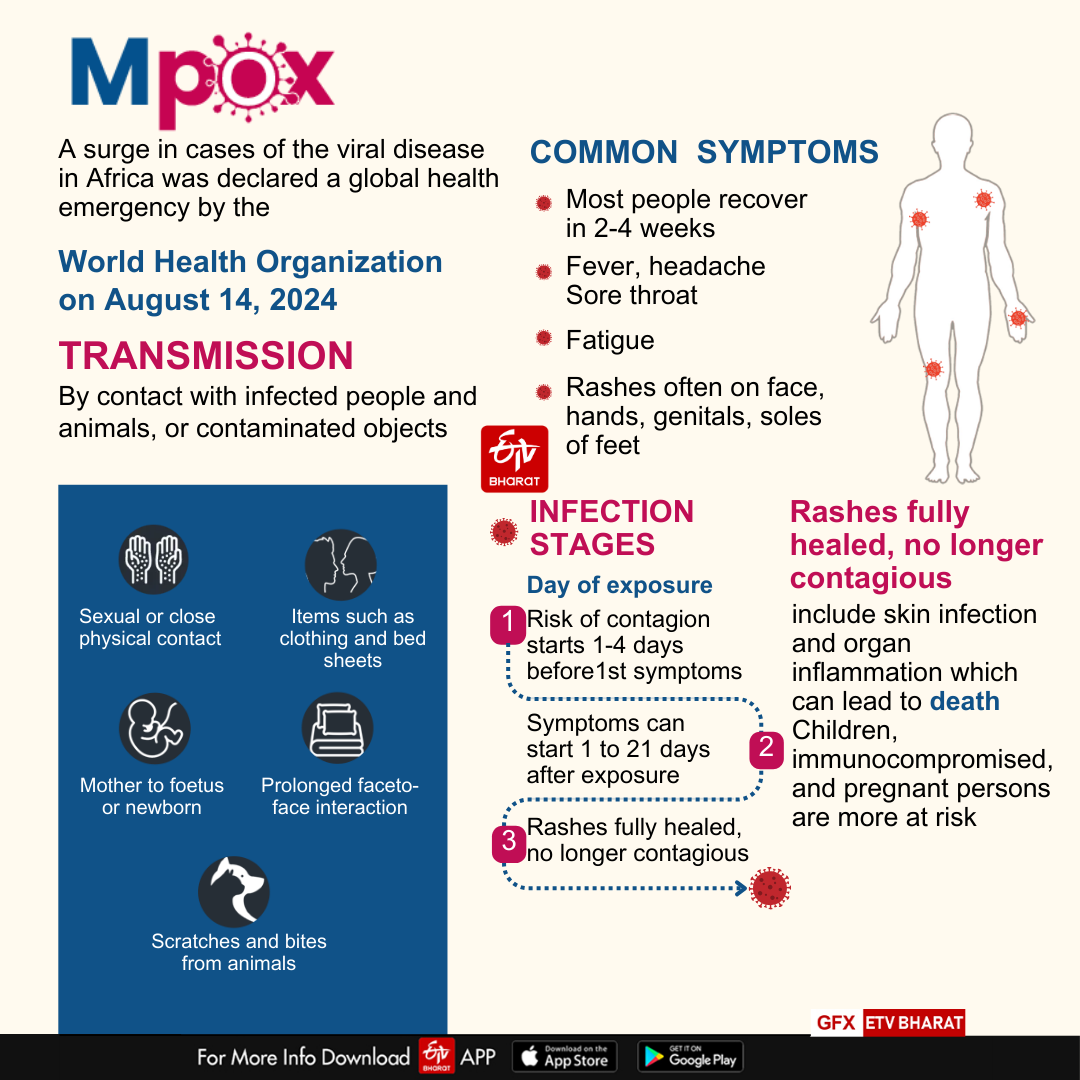
The disease was originally noted in humans in the Democratic Republic of Congo in 1970 and remained mostly confined there till 2022 when it started spreading to other countries. WHO first declared it a global public health emergency in July 2022 but withdrew that in May 2023 when the number of newly infected persons in Africa decreased. However, due to evidence of fresh spread across Africa and to countries on other continents and the emergence of a new strain of the virus, WHO again declared a public health emergency on August 14, 2024. Mpox belongs to the same family of orthopox viruses as chicken pox and smallpox.
While smallpox was globally eradicated by 1980, chickenpox is still around to infect humans, mostly children. A distinguishing feature is the appearance of skin lesions on palms and soles in Mpox, unlike in chickenpox. Mucous membranes of the mouth and anus as well as genitalia can be affected, swollen, painful lymph nodes are another characteristic feature. Patients develop fever, muscle pains and characteristic skin lesions which evolve through several stages till they are shed as dry scabs which can infect others. Infection is usually through bodily contact with an infected person, by touch or sexual activity. Droplets of sputum can also infect if a person is standing close to an infected person.
Recovery is usually the rule, though the severity of illness and death rates differ between the two strains of the virus. Prior immunisation with smallpox vaccine confers immunity against Mpox but such protection will not be available to Indians born after 1978 as the national smallpox vaccination programme was stopped after that. Elderly persons, malnourished children, pregnant women and persons with pre-existing health disorders are more likely to experience severe disease and complications.
Case detection is easier for Mpox than for Covid-19, because of the typical skin lesions. People must be encouraged to report to a healthcare facility if they notice vesicles (eruptions which are small fluid-filled sacs) developing on the skin. People who have Mpox must not face stigma so that they can seek care without hesitation. Those who develop Mpox need to be isolated from other persons till fully free of skin lesions and treated symptomatically.
While some anti-viral drugs have been developed, a recent drug trial failed to show benefit. Two types of vaccine are available but have not been distributed globally. Since the majority of infected persons recover without serious complications, many countries have not yet initiated a mass vaccination programme. When that starts, persons born after 1978 must be prioritised. Those who wish to protect themselves from infection, while meeting an infected person or while travelling, should avoid physical contact and frequently wash hands. Facing an infected person in close proximity must be avoided, even while conversing. Safe sexual behaviours are advocated, as men having sex with men or with female sex workers have been found to be at high risk. Unlike Covid-19, the Mpox virus does not spread by aerosols. So, masks are not advocated, unless a person is in close and frequent person with an infected person.
In India, around 30 sporadic cases were reported between July 2022 and March 2024. No new cases have been reported during the recent global spread. Europe and West Asia, through whose crowded airports travellers from Africa travel in large numbers are at higher risk than India. The likelihood of a large outbreak in India is small because we do not see such transit passengers. Unlike Covid-19, the monkeypox virus does not spread through airborne transmission via aerosols. However, we must keep our public health systems on alert and closely watch the global situation to see if the infections surge or subside.
There is no need to panic but our health systems must be prepared to respond to the increasingly frequent threat of zoonotic infections. The resurgence of Mpox is yet another reminder of the fact that humans have created the conditions for viruses confined to forests come into human populations when wild animals are forced to migrate due to deforestation.
(Disclaimer: The opinions expressed in this article are those of the writer. The facts and opinions expressed here do not reflect the views of ETV Bharat)



