Cervical cancer is the second most common cancer among Indian women, claiming over 67,000 lives annually, second only to breast cancer. It accounts for 17% of all cancer deaths among women aged 30 to 69 years, said a report published in the Lancet journal. But what lies behind these staggering numbers, and why does this disease continue to persist despite being largely preventable?
What Is Cervical Cancer?
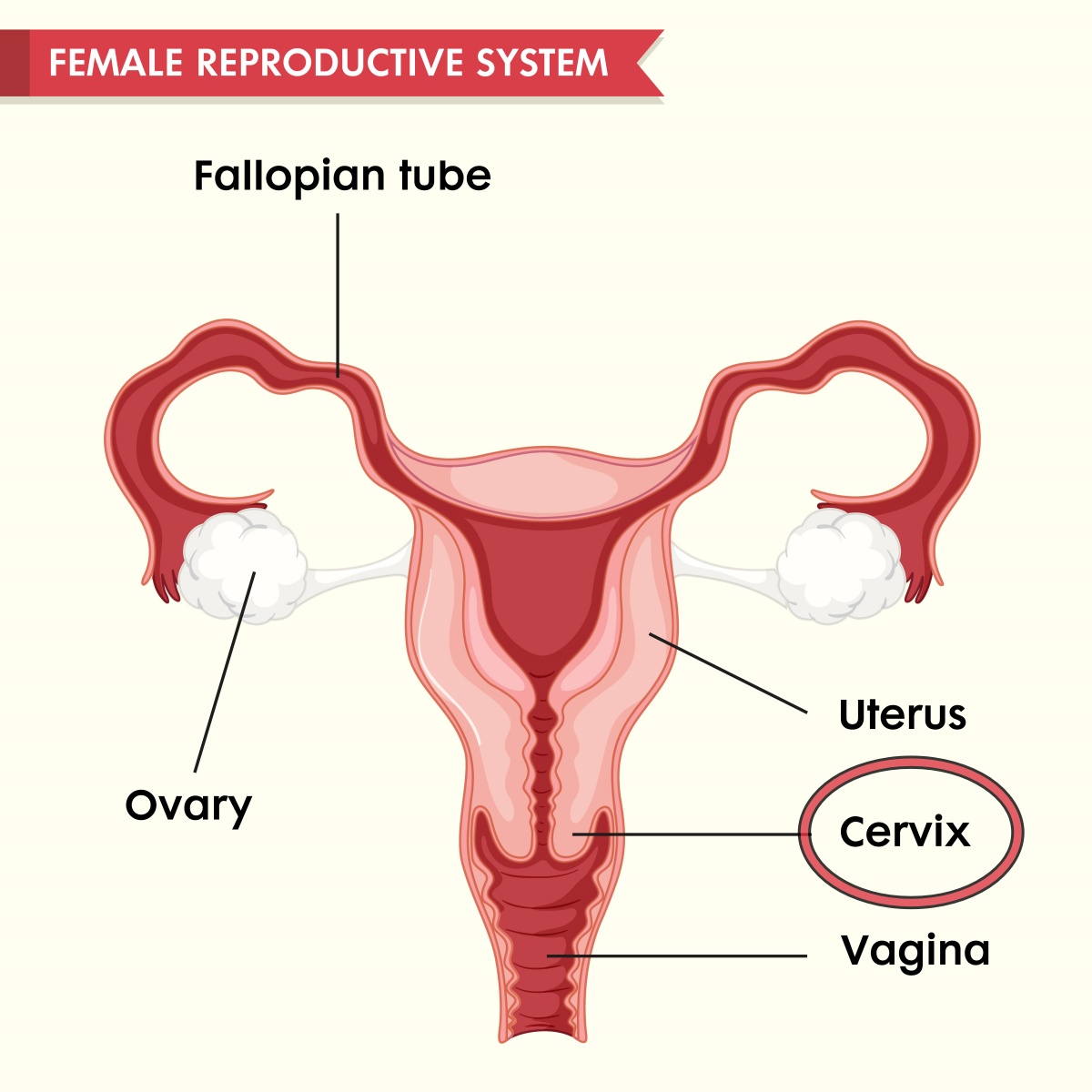
It is a type of cancer that starts in the cervix, which is the lower part of the uterus (womb) that connects to the vagina. It happens when abnormal cells grow uncontrollably on the cervix. If not detected and treated early, cervical cancer can spread to other parts of the body and become life-threatening.
However, it’s often preventable through HPV vaccination, regular screening tests like Pap smears, and early treatment of any abnormal changes in cervical cells.
The HPV Connection
At the core of cervical cancer lies high-risk human papillomavirus (HPV), a sexually transmitted infection. According to Dr. Aravind Badiger, Technical Director at BDR Pharmaceuticals, chronic HPV infection, particularly by types 16 and 18, is the primary culprit. Vaccines such as Gardasil and Cervarix have proven highly effective in preventing HPV infections, yet their uptake in India remains alarmingly low.
“Cultural factors, lack of awareness, and resource limitations mean vaccine coverage is still inadequate, especially in rural areas,” says Dr. Badiger. While immunization programmes targeting young girls (before they become sexually active) are the global norm, India faces the challenge of making these programmes accessible and widely accepted.
The Birth Cohort Effect
The rise in cervical cancer cases isn’t simply about genetics. “A birth cohort effect (an increase in risk among women born after 1960) suggests a generational shift influenced by lifestyle and environmental factors,” says Dr. Badiger. Obesity, metabolic syndrome, sedentary lifestyles, and even stress exacerbate this risk.
“Poor diet and exposure to tobacco compound the problem, since these factors weaken the immune system and increase inflammation,” says Dr. Reshma Puranik, Consultant Medical Oncologist at Ruby Hall Clinic in Pune.
The link between lifestyle and cancer prevention cannot be overstated. Addressing key lifestyle factors can lower the risk of cervical cancer significantly. “The best thing an individual can do is to quit smoking,” says Dr. Puranik. “Tobacco negatively affects almost every organ and weakens the immune system, leaving the body vulnerable to infections like HPV. Combine this with a balanced diet rich in antioxidants and regular exercise, and you create a natural defense against chronic diseases.”
Dr. Puranik also considers stress management as a crucial pillar of health. Chronic stress disrupts hormonal balance and destabilizes immune function. Activities like mindfulness and meditation can help offset these harmful effects.
While cities see increasing awareness, rural areas remain a challenge. Many women do not access healthcare until symptoms (such as abnormal bleeding or pelvic pain) become severe. By then, cervical cancer is often in advanced stages, making treatment more difficult and less effective.
What Are The Solutions?
Dr. Badiger underscores the need for collaborative efforts between healthcare providers, policymakers, and pharmaceutical companies:
“The industry must focus on making vaccines more affordable and accessible, especially for underserved communities. Alongside vaccines, early diagnostic tools such as low-cost HPV tests are essential for catching the disease at its pre-cancerous stage.”
Diagnostics (including molecular tests) have improved access to early detection. Technologies like cryotherapy and Loop Electrosurgical Excision Procedures (LEEP) can remove abnormal tissue before it progresses to cancer. However, these advancements must be paired with nationwide campaigns to educate women about the importance of routine screenings and vaccinations.
“Affordable diagnostics and mobile health camps can help bridge the urban-rural gap,” he says. With targeted interventions, such as community-led vaccination drives, India could significantly reduce cervical cancer’s mortality rate.
For those already diagnosed, advancements in immunotherapy, targetted therapies, and enhanced chemotherapy regimens are offering new hope. These treatments focus on reinforcing the immune system to target cancer cells more effectively and with fewer side effects than traditional methods. However, the key remains prevention and early detection, as these strategies are far more effective than treating advanced cancer.
References:
https://www.thelancet.com/journals/lansea/article/PIIS2772-3682(23)00156-7/fulltext
https://pmc.ncbi.nlm.nih.gov/articles/PMC5234166/
https://pubmed.ncbi.nlm.nih.gov/24217555/
(Disclaimer: The information provided in this health article is for general informational purposes only and is not intended as medical advice. It is not a substitute for professional healthcare consultation, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.)
Read more:



